The Tragic History of Tainted Blood: A Warning for Today!
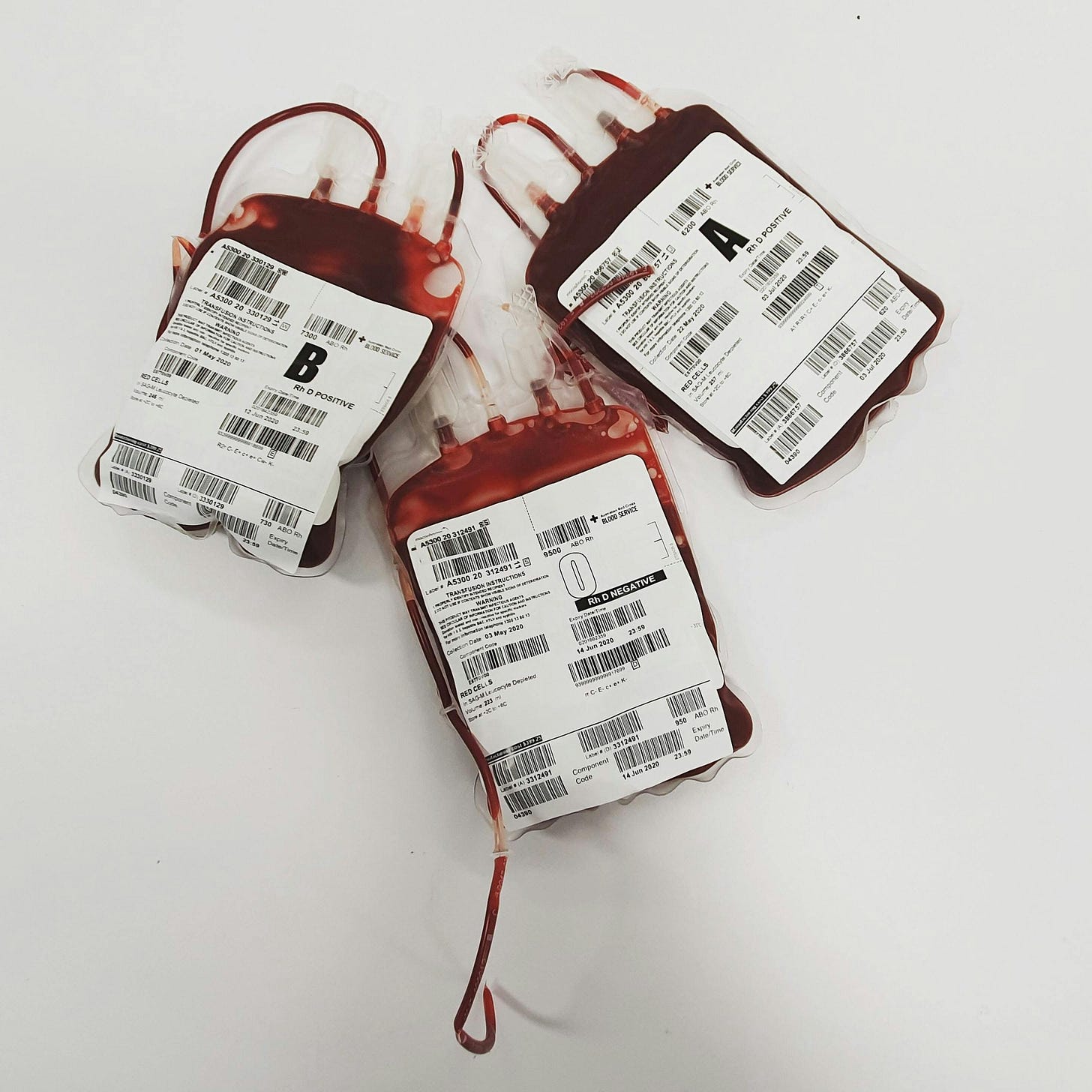
The history of the blood supply is a sobering one. From the 1980s onward, thousands of people in the United States, the United Kingdom, and Australia were unknowingly exposed to deadly viruses, including HIV and Hepatitis, through contaminated blood transfusions. What was once a symbol of trust—medical professionals’ promise to care for their patients—became a nightmare for many who received blood products that had been tainted due to lack of proper screening and negligence.
This dark chapter in medical history, which continues to impact survivors and their families today, serves as an urgent reminder: we must ensure that the blood we receive is safe and uncontaminated. And yet, as new threats emerge in the form of synthetic mRNA and gene-editing technologies, we are once again faced with the uncomfortable question of whether the medical system is doing enough to safeguard our blood supply.
The HIV and Hepatitis C Crisis: A Failure to Protect Patients
In the 1980s, the blood supply was severely compromised by the presence HIV, which caused the global AIDS epidemic. Hemophiliacs, who relied on blood-clotting factors to manage their condition, were among the hardest hit. These individuals received contaminated blood products that were unknowingly infected with the HIV virus. At the time, blood banks did not have the necessary testing protocols in place to identify HIV, and it wasn’t until the early 1980s that blood banks began screening for the virus.
The tragedy did not stop with HIV. Alongside it, Hepatitis B and Hepatitis C were also transmitted through contaminated blood products. Many hemophiliacs and patients receiving blood transfusions contracted these viruses, leading to chronic liver disease, cirrhosis, and in many cases, death. While some countries acted quickly to implement better testing, others were slower to respond, and lives were lost as a result.
The United Kingdom: A Scandal of Negligence
In the United Kingdom, the blood contamination crisis took on a more public dimension with the notorious “Tainted Blood Scandal.” Between the 1970s and 1980s, British hemophiliacs were given blood products infected with HIV and Hepatitis C, in some cases causing widespread illness and death. The blood was often sourced from foreign donors, particularly in the U.S., where screening was lax, and paid donors were common.
The scandal grew when it was revealed that government and health authorities had been aware of the dangers of imported blood but did little to stop the practice. In fact, even after it became clear that the blood was contaminated, the public was not informed, and patients continued to receive the infected products. This resulted in over 5,000 individuals contracting HIV and Hepatitis C in the UK alone.
A public inquiry, known as the Archer Inquiry, was launched in 1996 to investigate the scandal, but it wasn’t until much later, in the 2000s, that victims and their families began to receive proper compensation and acknowledgment. Many survivors of the contaminated blood scandal in the UK, as well as their families, continue to fight for justice, with calls for a full apology from the government and better support for those affected.
Australia’s Delay: The Price of Inaction
Australia’s experience with tainted blood was equally tragic, but the delay in testing for Hepatitis and HIV made the situation even worse. Like many countries, Australia relied heavily on imported blood products, particularly from the United States. The country’s decision to wait until the late 1980s to begin more rigorous testing for Hepatitis led to a significant number of hemophiliacs and others who received transfusions contracting the disease.
What set Australia apart, however, was the public outcry that followed. In the wake of the contaminated blood scandal, hemophiliac patients and their families sought justice for the harm that had been done. The Australian government eventually established a compensation program for those affected, but the process was slow, and many families were left struggling to care for loved ones who the virus had impacted.
A Lack of Accountability: How the System Failed
One of the most disturbing aspects of the tainted blood scandals in all three countries was the lack of accountability. Blood banks, health authorities, and pharmaceutical companies were slow to act, even after evidence surfaced that blood products were contaminated. In some cases, there was even evidence of a cover-up. Medical professionals were not given the information they needed to protect their patients, and patients were not told of the risks involved in receiving blood transfusions.
It wasn’t until the mid-1980s that widespread screening for HIV and Hepatitis began, but by then, many lives had already been irreversibly affected. The victims of this medical negligence were forced to endure not only the physical suffering caused by these deadly viruses but also the emotional pain of betrayal by a system they trusted.
The Need for Transparency and Accountability in Today’s Blood Supply
The tainted blood scandals of the 1980s and 1990s serve as a stark reminder of the importance of safety, transparency, and accountability when it comes to blood products. The failure to protect patients then was catastrophic, but the consequences of ignoring these issues today could be even more profound.
As the medical industry pushes forward with gene therapies and the introduction of synthetic mRNA into the human species and biological products, we are once again faced with the need to ask: Are we sure our blood is safe? How can we be certain that the blood we receive doesn’t contain genetic modifications or other untested technologies?
The public deserves transparency. Just as we have the right to know what’s in our food, we should have the right to know what’s in our blood. We can no longer afford to trust blindly in the medical system. We must advocate for a blood supply free from contamination, whether that contamination comes from viruses, synthetic mRNA, or gene-editing technologies.
Call to Action
The lessons from the past are clear: we must be vigilant, and we cannot simply trust the science or authorities to make swift and decisive action for our safety. We must protect our blood supply from the dangers of contamination, and we must demand accountability from the institutions responsible for our health. Join Impact Reconciliation in our mission to build an mRNA-free blood supply and ensure that everyone has access to clean, safe blood when they need it most.
Just like in the years before with HIV and Hepatitis, there was a waiting period before screening was introduced. Now, we can analyze blood to see if mRNA vaccines have been added to it through injection or transmission. Visit Impact Reconciliation to learn more.